Last week, the World Health Organization, or WHO, determined that a surge of mpox cases in several African countries constitutes a “public health emergency of international concern.” Here’s what this means for you.
What is monkeypox?
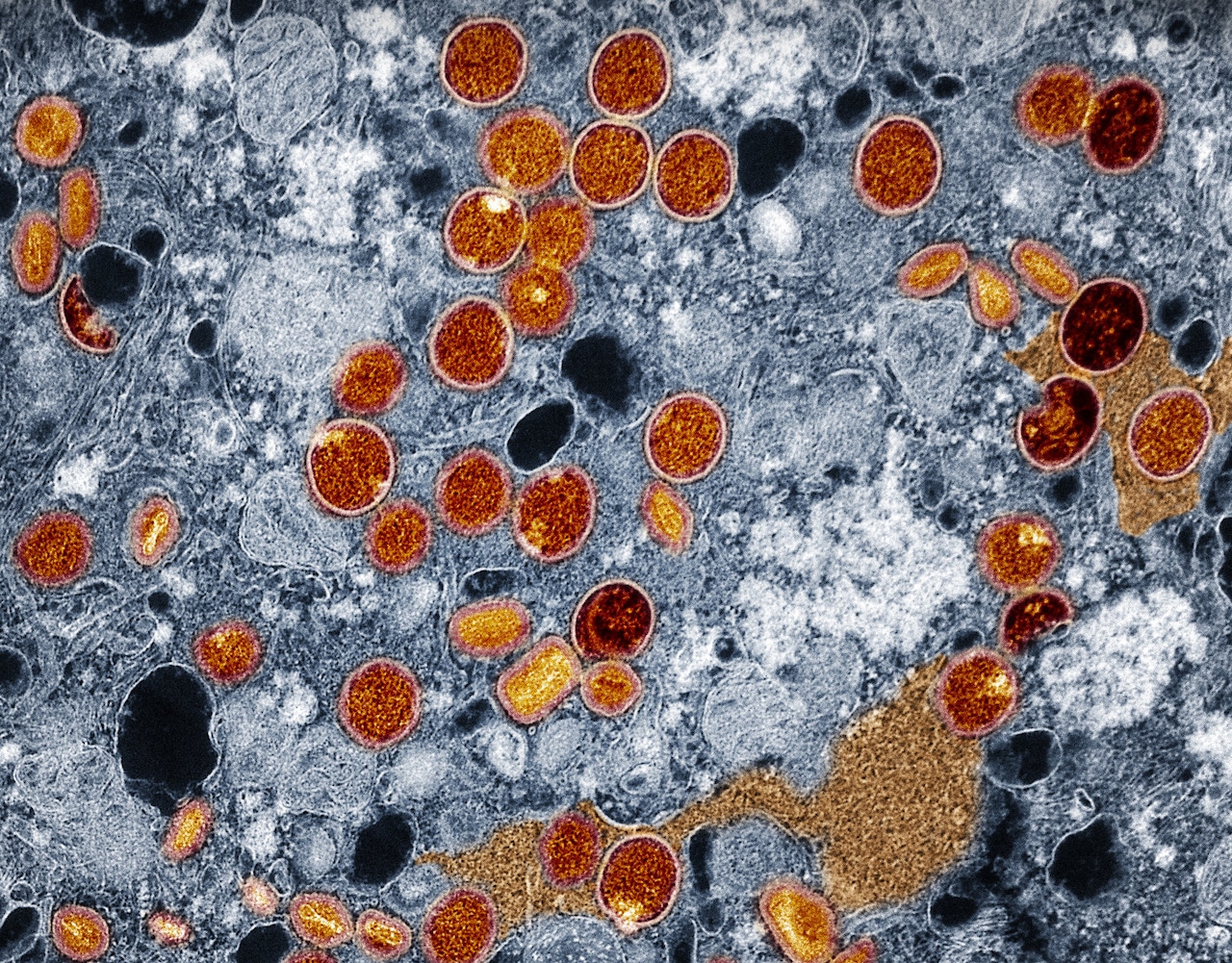
Mpox, formerly known as monkeypox, is caused by a virus similar to the smallpox virus, according to the Centers for Disease Control (CDC). People with mpox often get a rash, but most cases are not life-threatening.
Mpox is endemic, i.e. found regularly, in parts of Central and West Africa, according to the CDC. It was originally called monkeypox because it was first discovered in monkeys in 1958, though its animal origin remains unknown.
There are two clades of mpox — clade I, which is endemic to Central Africa, and clade II, which is endemic to West Africa, according to the CDC. Clade I is deadlier and has historically killed up to 10% of infected people. Clade II led to the global mpox outbreak in 2022.
What is a PHEIC?
A public health emergency of international concern, or PHEIC, is defined by international health regulations as a public health crisis that is serious, sudden, unusual or unexpected; could impact countries around the world and may require immediate international action, according to the WHO.
The WHO’s director-general can declare a PHEIC after a committee of international public health experts meet to evaluate the situation and determine whether the situation rises to this crisis level.
What happened last week?
A WHO committee met last week and recommended a PHEIC be declared in response to an mpox outbreak in the Democratic Republic of the Congo (DRC) that has spread to neighboring countries, according to a press release from the WHO. The outbreak is due to a new strain of mpox called clade 1b, which emerged in the DRC last year and has been spreading through “sexual networks.”
The number of clade 1b cases reported in the DRC so far this year has already exceeded last year’s total, with more than 15,600 cases and 537 deaths, according to the WHO. Additionally, cases of the new strain are now beginning to appear in countries neighboring the DRC.
In the past month, more than 100 laboratory-confirmed cases of clade 1b have been reported in Burundi, Kenya, Rwanda and Uganda — none of which reported cases before, according to the WHO. Experts also believe the true number of cases is likely far higher than the number of confirmed cases.
“The emergence of a new clade of mpox, its rapid spread in eastern DRC, and the reporting of cases in several neighbouring countries are very worrying,” Ghebreyesus said in an Aug. 14 press release. “On top of outbreaks of other mpox clades in DRC and other countries in Africa, it’s clear that a coordinated international response is needed to stop these outbreaks and save lives.”
What happens now?
WHO Director-General Tedros Adhanom Ghebreyesus is now expected to make temporary recommendations to countries on how to deal with the outbreak, the WHO said. The director-general has also started the process of listing mpox vaccines for emergency use, which will accelerate vaccine access for lower-income countries.
The WHO is in the process of working with countries and vaccine manufacturers to acquire vaccine donations, according to the organization. It is also coordinating with its international partners to facilitate access to other healthcare tools that can help prevent and treat mpox.
So far, the WHO has released $1.45 million in emergency money to scale up international mpox surveillance, preparedness and response efforts, but it anticipates that it will ultimately need $15 million to achieve its goals, the WHO said. The organization may release more emergency money in coming days and will be appealing to donors for additional funds.
What are the symptoms of mpox?
People with mpox often get a rash on their hands, feet, chest, face, mouth or near their genitals, according to the CDC. The rash may look like pimples or blisters and be itchy or painful.
Other symptoms of mpox include fever, chills, swollen lymph nodes, exhaustion, muscle aches, headache, sore throat, congestion and coughing, according to the CDC. Some people experience all the symptoms of mpox, while others only experience a few.
Mpox symptoms typically appear within 21 days of exposure to the virus, and flu-like symptoms often precede a rash by several days, according to the CDC. Mpox also has an incubation period of three to 17 days, during which a person will not have symptoms and may feel fine.
Children less than a year old and people with severely weakened immune systems, a history of eczema or who are pregnant are more likely to develop severe illness as a result of a mpox infection, according to the CDC.
How does mpox spread?
Mpox spreads through direct contact with infected people or animals, including skin-to-skin contact with an mpox rash or contact with the bodily fluids or waste of an infected person or animal, according to the CDC. It is often spread through touching an infected person or pet, hunting or trapping infected wild animals, sexual contact with an infected person, scratches or bites from infected wild animals or from a pregnant person to their unborn child.
Mpox can also spread through the touching of objects and surfaces that an infected person or animal has come into contact with, such as clothing, bedding, towels, fetish gear or sex toys, according to the CDC. The virus is not known to spread through water in pools, hot tubs or splash pads.
A person with mpox can spread the virus from the time their symptoms start to when their rash has fully healed, according to the CDC. Evidence suggests that people can spread mpox days before their symptoms appear, but that people who never show symptoms are not infectious.
How do I keep from becoming infected?
- Get vaccinated if you are among those recommended for vaccination by the CDC
- Avoid close contact with people or animals who have an mpox-like rash
- Avoid events and places where there is often direct, skin-to-skin contact with others, such as music festivals, raves, parties and clubs
- Wash your hands frequently
- Engage in CDC-recommended mpox-safe sex practices
- Do not share eating utensils or cups with a person with mpox
- Do not handle or touch the bedding, towels or clothing of a person with mpox
- If living with someone with mpox, disinfect your home as recommended by the CDC
Anyone who thinks they have been exposed to mpox should monitor themselves for symptoms for three weeks after their last exposure, according to the CDC. Anyone who has been exposed to the virus and exhibits symptoms, especially a rash, should contact their healthcare provider to get tested for mpox.